UCLA's cutting-edge Duchenne muscular dystrophy research funded by California's stem cell agency
Scientists at the UCLA Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research and Center for Duchenne Muscular Dystrophy at UCLA have received funding from California’s stem cell agency for the next phase of cutting-edge stem cell gene therapy research that could eventually produce a treatment for Duchenne muscular dystrophy, which affects approximately 1 in 5,000 boys in the U.S. and is the most common fatal childhood genetic disease.
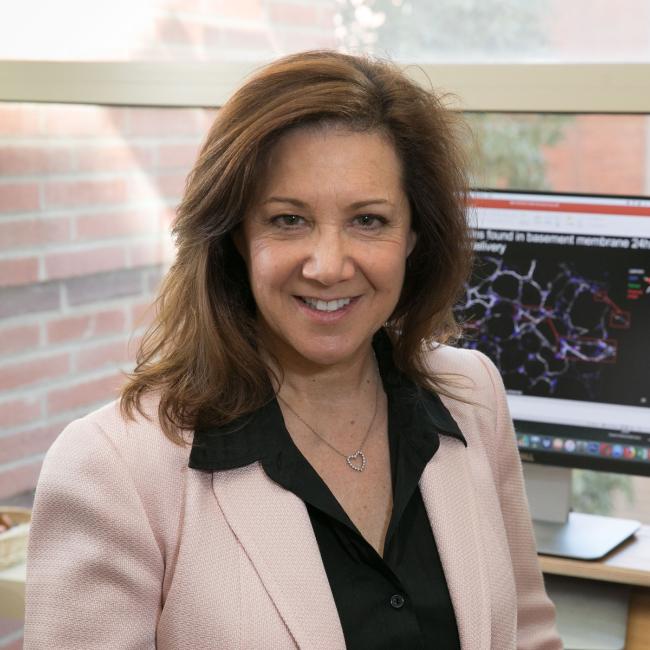
The grant, awarded to scientists April Pyle, Melissa Spencer and Huan Meng, totals $2,150,400. The decision to fund the research was made during today’s meeting of the California Institute for Regenerative Medicine’s governing board.
The researchers will utilize a stem cell gene editing technology called CRISPR/Cas9 in two different approaches to correct the genetic mutations that cause Duchenne. The two approaches will use nano-scale particles that will be tested in mice over the course of the two-year project to determine if the methods are viable for use in a clinical setting in the future.
Duchenne typically occurs through mutations in a gene called dystrophin, which makes a protein with the same name. In people without the disease, the dystrophin protein helps strengthen and connect muscle fibers. There are hundreds of mutations in the dystrophin gene that can lead to the disease, but in 60 percent of people with Duchenne, their mutation occurs within a specific hot spot of the gene.
Duchenne mutations cause abnormally low production of the dystrophin protein, which in turn causes muscles to degenerate and become progressively weaker. Symptoms usually begin in early childhood; patients gradually lose mobility and typically die from heart or respiratory failure around age 20. Some current medications can treat the disease’s symptoms but none can stop the progression of the disease or significantly improve patients’ quality of life. There is currently no way to reverse or cure Duchenne, which is the most common and severe form of more than 30 forms of muscular dystrophy.
Previous research from the Pyle and Spencer laboratories showed that the gene editing technology CRISPR/Cas9 could correct Duchenne mutations in induced pluripotent stem cells created from patients with the disease, and that those stem cells could be turned into muscle cells that restore production of the human dystrophin protein in preclinical research models.
CRISPR/Cas9 is a naturally occurring reaction that bacteria use to fight viruses. In 2012, scientists discovered they could adapt the process to make cuts in specific human DNA sequences. One part of the CRISPR/Cas9 system acts like a navigation system and can be programmed to seek out a specific part of the genetic code — a mutation, for example. The second part of the system can cut mutations out of the genetic code, and in some cases can replace the mutation with a normal genetic sequence.
Induced pluripotent stem cells, or iPS cells, are created by taking cells from a patient – typically skin cells – and reprogramming the cells in a dish in the lab. This reprogramming method creates ‘pluripotent’ stem cells that can become any type of human cell while also maintaining the genetic code from the person they originated from.
“Once we developed the CRISPR/Cas9 platform for Duchenne mutations, we knew our next challenge would be to correct the muscle stem cells that reside throughout approximately 40 percent of the body that is made of muscle tissues,” said Pyle, associate professor of microbiology, immunology and molecular genetics, member of the Broad Stem Cell Research Center and principal investigator for the newly funded research.
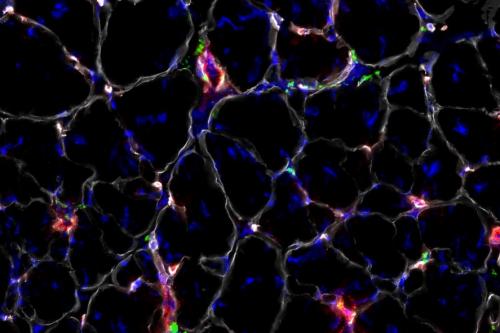
Muscle stem cells reside in skeletal muscle, have the ability to make muscle cells and are responsible for replenishing muscle tissue throughout a person’s life. In people with Duchenne, this natural regenerative process does not occur effectively over time due to the mutations in the dystrophin gene.
Building on previous research, Pyle explained that the next challenge is finding a way to either correct the Duchenne mutation in the muscle stem cells throughout the body, or deliver muscle stem cells that have been corrected in the lab and ensure they reach the right places in the body. Any approach that might result in a practical treatment needs to be delivered system-wide, said Pyle.
Using nanoparticle technology to correct genetic mutations
Pyle and Spencer are partnering with Meng, an assistant professor of nanomedicine, to come up with two potential systemic delivery methods using specialized nano-scale particles, or nanoparticles. The nanotechnology component of the research will be performed in the California NanoSystems Institute.
Nanoparticles are microscopic particles that can be used to transport information to cells by packaging materials that send or deliver messages to the cells. For the newly funded Duchenne research, Meng will create different modifications to nanoparticles made of a porous chemical compound that allows for encapsulation, binding and release of materials inside cells.
The first method will deliver the CRISPR/Cas9 gene editing technology previously developed by Pyle and Spencer directly to muscle stem cells in mice that have been engineered to have a human Duchenne mutation in the hot spot of the dystrophin gene. The team plans to encapsulate the CRISPR/Cas9 technology in the nanoparticles and inject the nanoparticle package intravenously into mice. The researchers intend to monitor how well the nanoparticles deliver the CRISPR/Cas9 technology to muscle stem cells in the mice and measure how well the technology corrects the Duchenne mutations.
The second method is a two-step approach. The team will inject nanoparticles that contain a chemoattractant intravenously into mice. The chemoattractant is a special protein that attracts cells of a particular type to the correct location in the body. Then, the scientists will inject human muscle stem cells that have been corrected in the lab with the CRISPR/Cas9 technology to remove Duchenne mutations. The researchers anticipate the corrected muscle stem cells will migrate towards the chemoattractants that are dispersed in muscle throughout the body and, once there, repopulate the muscle with muscle stem cells that are free of Duchenne mutations.
“We are excited to use the latest high-tech approaches to further our research and hopefully someday create a treatment for Duchenne,” said Spencer, professor of neurology in the UCLA David Geffen School of Medicine, co-director of the Center for Duchenne Muscular Dystrophy at UCLA and member of the Broad Stem Cell Research Center. “We’re thankful that the California Institute for Regenerative Medicine has funded our work.”
Spencer explained that the method is likely 10 years away from being tested in people and the necessary steps need to be taken to maximize safety while quickly bringing a therapeutic treatment to patients in clinical trials.
The CRISPR/Cas9 platform for Duchenne developed by the UCLA scientists is not yet available in clinical trials and has not been approved by the FDA for use in humans.