UCLA bioengineers show key step toward efficient and nonrandom cell reprogramming
UCLA bioengineers and colleagues have discovered and detailed a key step in cell reprogramming for safe drug testing and other personalized disease therapy.
Cell reprogramming is an emerging technology that can convert target cells pre-programmed with a biological function into malleable stem cells, or another cell type, with an entirely different function.
The research was recently published in Advanced Science and could play an important role in personalized medicine and the discovery of new drugs.
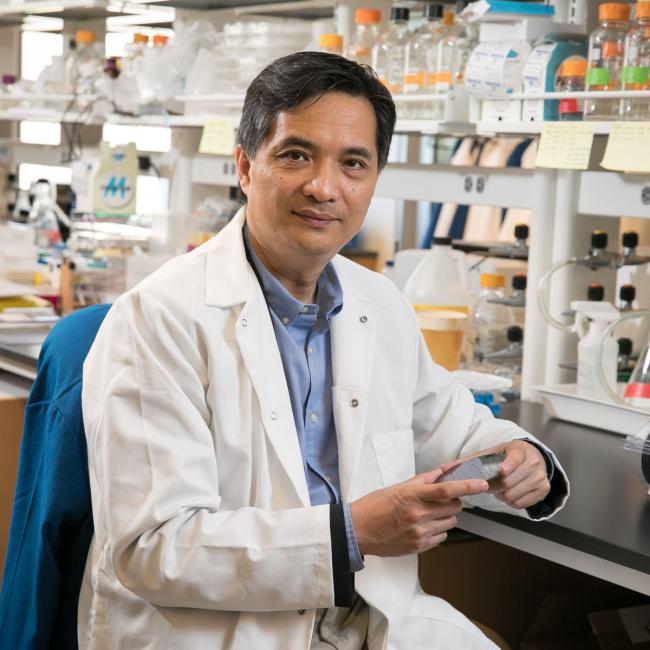
“Cell reprogramming is one of the most exciting advancements in biotechnology in the past 20 years,” said study leader Song Li, professor and chair of the bioengineering department at the UCLA Samueli School of Engineering and member of the Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research at UCLA. “It’s the cellular equivalent of wiping your computer’s memory clean and replacing it with new software. This is a very powerful process in biotechnology that could lead to therapies based on patients’ own cells and their own genes.”
Since these reprogrammed cells would have the person’s own unique genetic makeup, drug tests can be performed outside the body.
The advance may lead to multiple applications. For example, a person’s skin cells could be grown in a Petri dish and reprogrammed into neuronal cells — electrically excitable brain cells that communicate with other cells via specialized connections called synapses. Since these reprogrammed cells would have the person’s own unique genetic makeup, drug tests can be performed outside the body. Medications to treat brain diseases could be tested on the reprogrammed cells to see if they work well or may cause an adverse reaction. In addition, a person’s skin cells could be reprogrammed into heart muscle cells that would be an exact genetic match for a transplant to avoid tissue rejection.
“However, while very promising, the conversion rate into reprogrammed cells is not yet efficient enough for these applications,” added Li, who also holds an appointment in the David Geffen School of Medicine. “In this research, we have unraveled a key molecular mechanism in the process, which we hope will ultimately play a major role in the development of real therapies.”
The researchers also wanted to determine if reprogramming happens to random cells, or if there are “elite” cells primed for conversion. They discovered it’s the latter.
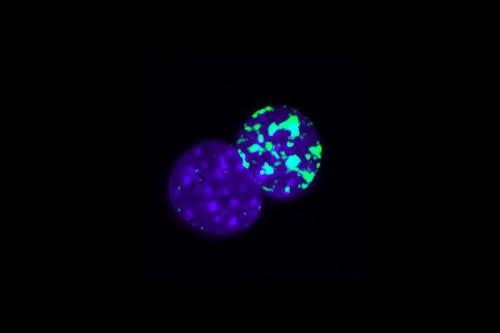
In their experiments, the researchers used skin cells from mice and reprogrammed them into neuronal cells. While a cascade of different molecular mechanisms can lead to reprogramming, researchers found that a critical step involves inducing a phenomenon called asymmetric cell division, or ACD.
In normal cell division, a cell divides into two daughter cells identical to the original. During ACD, which has thus far only been observed in stem cells, one daughter cell remains a stem cell while the other will have a biological function, such as a neuron or muscle cell.
The experiments showed that during cell reprogramming, one daughter cell following ACD was primed for conversion. Whereas when ACD was disallowed, the efficiency of cell conversion from skin cells to neurons was much lower.
Another key finding pertains to DNA-strand replications. Before cells divide, their DNA molecules are replicated, creating two of each strand — an original and a new copy. The researchers observed during ACD that the daughter cells with the new copies were the ones primed for reprogramming into neurons.
“We now know that there is a definite and efficient method — asymmetric cell division — to generate cells primed for reprogramming,” Li concluded.
In addition to Li, other UCLA authors include lead author Yang Song, who along with fellow bioengineer Jennifer Soto and others are members of Li‘s Cell and Tissue Engineering Lab; and Qin An and Guoping Fan from the Department of Human Genetics. Other authors are from Brigham and Women’s Hospital in Boston, Harvard Medical School and Chongqing University in China.
The authors were supported in part by a UCLA Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research Innovation Award, a grant from the National Institutes of Health, and a postdoctoral fellowship to Soto from the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the NIH under the Ruth L. Kirschstein National Research Service Award.