Scarring following heart attack causes unique genetic changes within the heart
UCLA researcher Dr. Arjun Deb, member of the Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research at UCLA, has discovered how heart scarring following a heart attack produces genetic changes that cause increased heart size and thickening.
Two of the main types of cells in the heart are cardiomyocytes, the heart’s muscle cells that beat to pump blood, and cardiac fibroblasts, which exist between cardiomyocytes and act as a scaffold that binds the cardiomyocytes together. Cardiac fibroblasts reside as single cells in between cardiomyocytes, but following a heart attack, cardiac fibroblasts migrate to the injured area and aggregate, which forms scar tissue. This migration and aggregation represent unique events in the life cycle of cardiac fibroblasts. Prior to Deb’s study, little was known about how changes in the spatial arrangement of cardiac fibroblasts following a heart attack affect the cells and overall heart health.
Deb’s study, published in the journal Circulation Research, has found that such changes in the spatial arrangement of cardiac fibroblasts profoundly affect the cells’ gene expression patterns and function.
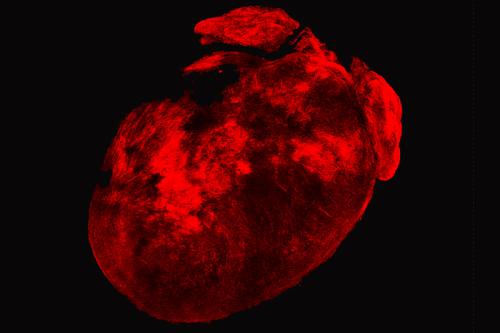
To investigate how post-heart attack changes in the spatial arrangement of cardiac fibroblasts affect the cells, the research team dissolved all the caridomyocytes in mouse hearts that had experienced a heart attack. A three dimensional scaffold of cardiac fibroblasts remained as well as areas of scarring where cardiac fibroblasts had aggregated. Examining this scaffold, the researchers observed that gene expression generated by aggregating fibroblasts in a 3-D pattern highly correlated with genes known to unfavorably affect heart function after a heart attack. Furthermore, aggregated cardiac fibroblasts secreted proteins that, when added to human stem cell-derived cardiomyocytes in laboratory dishes, increased heart muscle swelling and thickening.
“We found that the aggregated state of cardiac fibroblasts significantly changes the cells and causes subsequent consequences that are adverse for the healing heart,” said Deb, an associate professor of cardiology in the David Geffen School of Medicine at UCLA. “We also found that switching the cells out of an aggregated state reverses the negative genetic changes that are associated with poor heart health in humans; this means the system is highly dynamic and reversible, potentially providing us a therapeutic opportunity”
Deb and his team plan to continue to investigate how the aggregation of cardiac fibroblasts has implications for heart healing and if this information can help cardiologists find better treatments for heart scarring.
The study was funded by the National Institutes of Health, the Department of Defense, the Air Force Office of Scientific Research, the California Institute for Regenerative Medicine, UCLA Broad Stem Cell Research Center (BSCRC)-California NanoSystems Institute Planning Award and the BSCRC Rose Hills Foundation Research Award.
