A metabolic process in cancer cells could unlock a possible treatment for glioblastoma
Key Takeaways
- Glioblastomas are lethal brain tumors with few treatment options and a poor prognosis for most patients.
- A UCLA-led team identified a genetic alteration that occurs in 60% of people who are diagnosed with glioblastoma; that mutation disrupts the cancer cells’ metabolism.
- The discovery suggests that one possible approach to treat glioblastoma would be a therapy that targets the metabolic process in patients who have that genetic alteration.
A study led by researchers at the UCLA Jonsson Comprehensive Cancer Center has found that targeting a metabolic process in people with a specific genetic mutation could help treat glioblastoma, an aggressive brain cancer.
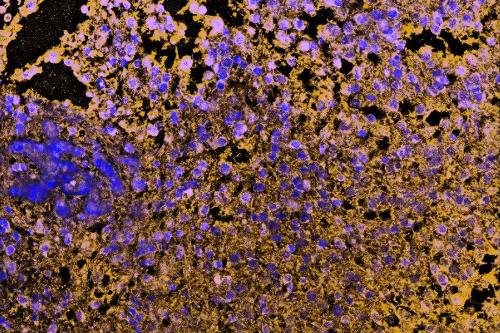
The genetic alteration — a deletion in a gene called CDKN2A — is present in about 60% of people who have glioblastoma. The mutation causes changes in the way lipids are distributed in cancer cells, which in turn makes the cancer cells vulnerable to being destroyed. The discovery, published in Cancer Cell, could suggest a path toward the development of targeted therapies that specifically target that vulnerability.
“Each patient’s tumor can have a unique combination of genetic alterations,” said David Nathanson, co-senior author of the study and an associate professor of molecular and medical pharmacology at the David Geffen School of Medicine at UCLA. “Because all of these tumors are different, we need to understand how certain genetic changes can affect tumor metabolism in order to identify potential targets for future treatments.”
Scientists believe that disrupting cancer cells’ metabolism — the way that they process energy and nutrients in order to survive, grow and invade healthy cells — could be one key to new and effective treatments.
Developing new ways to treat glioblastoma is imperative, said Nathanson, who also is a member of the Jonsson Cancer Center. Glioblastomas are lethal brain tumors that grow quickly, and currently there are few treatment options. The average lifespan of someone diagnosed with the brain tumor is just 12 to 15 months, and only about 5% of people diagnosed with glioblastoma are alive five years after their diagnosis. President Joe Biden’s son Beau and Senator John McCain both died from the disease.
Looking for possible patterns in the way the cancer cells process fats — which might indicate that they could be vulnerable to medicine — the researchers analyzed data from 84 glioblastoma tumors, 42 human cell lines and 30 mouse models of glioblastoma. They noticed some irregularities with CDKN2A, the gene that is mutated in a majority of people with glioblastoma.

They found that the gene rewires lipid metabolism to work in a different way than cells without that genetic alteration. And when the CDKN2A gene is missing, the way cancer cells process fats makes them more vulnerable to cell death, or ferroptosis.
The team then used a drug that targets this process and found glioblastoma cells with the genetic alteration in CDKN2A were highly susceptible to cell death, while the glioblastoma cells that did not have the genetic alteration were insensitive to the drug.
“We discovered that CDKN2A may be a key regulator of cancer cell metabolism, which has never before been shown in the context of cancer, even though it is deleted in other types of cancer,” Nathanson said. “Importantly, we found that CDKN2A deletion rewires lipid metabolism not just in our models but also in tumors from glioblastoma patients. This indicates that this metabolic vulnerability could one day be a target of therapy in glioblastoma patients.”
While there is no existing drug that could penetrate the brain to target the process studied by the UCLA scientists, the study provides strong rationale to develop one, Nathanson said.
Steven Bensinger, the Sherie and Donald Morrison Professor of Immunology and co-senior author of the study, said another important aspect of the work is that it could shed new light on how diet and other lifestyle factors could influence cancer progression and patients’ responses to therapy.
“Our data indicates that CDKN2A-deleted cancer cells shift the type of lipids used to build their cellular membranes, and that this difference can be exploited to kill tumors,” Bensinger said. “This opens up the exciting possibility that prescribing special diets containing the ‘wrong’ lipids could make them more susceptible to therapy or reduce tumor growth.”
The database of the 156 glioblastoma samples that the investigators analyzed is now available to researchers worldwide; the team has also expanded the number of samples in the database to more than 500, which the scientists hope will help them identify additional relationships between cancer-fighting genes and specific types of lipids used by brain cancer.
The study’s other co-senior author is Scott Dixon of Stanford University. The co-first authors are UCLA doctoral candidates Jenna Minami and Nicholas Bayley, and Danielle Morrow, who earned her doctorate from UCLA in 2021. Other co-authors are Elizabeth Fernandez, Jennifer Salinas, Christopher Tse, Henan Zhu, Baolong Su, Rhea Plawat, Anthony Jones, Alessandro Sammarco, Dr. Linda Liau, Thomas Graeber, Kevin Williams and Dr. Timothy Cloughesy, all of UCLA.
The study was funded in part by grants from the National Institutes of Health and the Department of Defense.