Four UCLA stem cell researchers awarded $12 million in grants to translate basic discoveries into therapies
The state stem cell agency today awarded four grants totaling $12 million to researchers with the Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research at UCLA to translate basic science into new and more effective therapies to regenerate bone and treat deadly brain cancers, spinal cord injuries and corneal disorders that result in blindness.
The Broad Stem Cell Research Center received more early translational grants than any other institution in this round of funding.
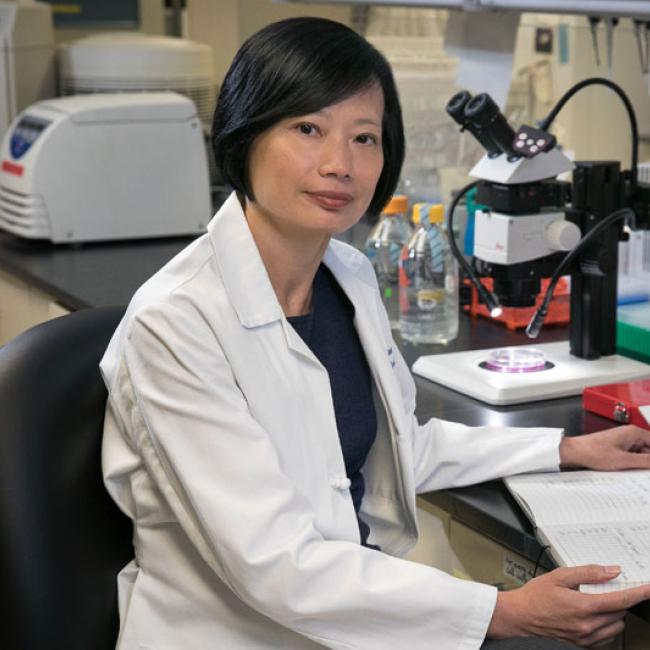
The Early Translational II grants, awarded by the California Institute for Regenerative Medicine (CIRM), went to Dr. Bruno Peault and Dr. Chia Soo, professors of orthopedic surgery ($5,391,560); Dr. Noriyuki Kasahara, a professor of digestive diseases ($3,370,607); Dr. Sophie Deng, an assistant professor of ophthalmology ($1,654,058); and Dr. Leif Havton, an associate professor of neurology ($1,614,441).
These awards are the second of what CIRM officials expect to be a 12- to 18-month award cycle for the translational research grants. The UCLA Broad Stem Cell Research Center considers the research funded by these awards critical to its mission to translate basic discoveries into clinical treatments. The funded projects are expected to either result in a candidate drug or cell therapy or make significant strides toward a drug candidate, which can then be developed for submission to the FDA for testing in clinical trials.
In all, CIRM today approved funding for 20 early translational grants totaling more than $68 million.
In their grant, Peault and Soo plan to use fat stem cells obtained through liposuction to form and regenerate bone, work that may result in a treatment that could help patients with back problems requiring spine fusion, bone fractures, herniated disks and, potentially, osteoporosis. If successful, their study could provide an alternative to traditional bone grafting.
The three-year study uses a novel combination of antibodies and cell sorting to prospectively isolate more purified stem cell populations from fat. The stem cells, called perivascular stem cells (PSC), are a breakthrough in stem cell technology because, unlike traditional fat-derived stem cells, PSC are not cultured for weeks before identification. The method allows patients to be treated much more quickly, yields more pure stem cell populations and decreases risk of contamination. The PSC would then be combined with a potent growth factor, NELL-1, that amplifies the ability of PSC to form bone. The mixture would then be implanted into patients to form bone.
Ideally, the fat would be taken by liposuction from the patient needing bone regeneration to avoid rejection that could result if the fat was taken from someone else. Peault and Soo hope to show that the rapidly isolated PSC can form bone better than conventional, culture-derived fat stem cells.
In his project, Kasahara seeks to use a replication-competent retrovirus that will only infect rapidly dividing cancer cells and transform the tumor cells themselves into virus producing cells in an effort to develop a new and more effective therapy to treat deadly glioblastomas.
Modified viruses can be used to infect tumor cells and make anti-tumor proteins. Most researchers use viruses – known as replication-incompetent - that can infect and modify the tumor cell it enters but cannot replicate itself to infect malignant cells surrounding the original infected cell. Use of a replication-incompetent virus is considered safe because no additional virus, which potentially could get out of control, is generated inside the tumor. However, such therapies have been shown only limited benefit, presumably because too many tumor cells remain uninfected.
Newer approaches focus on the use of replication-competent viruses, transforming the tumor cell itself into a virus-producing cell that attacks malignant cells and leaves the normal brain cells alone. Usually, a therapeutic virus is injected into the tumor. However, that would not target malignant cells that have diffused to other areas of the brain. Kasahara proposes using a type of adult stem cell called a mesenchymal stem cell (MSC) as a delivery system for the replication-competent retrovirus. MSCs have been shown to have natural tumor-homing abilities and can migrate to the diffuse tumor cells as well as penetrate into the interior of the primary tumor. Kasahara hopes to engineer the MSCs into "aircraft carriers" that release tumor-selective viruses, which can spread suicide genes from one cancer cell to another.
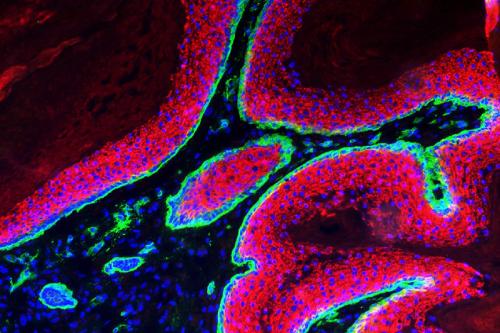
In her study, Deng hopes to regenerate functional human corneal epithelial progenitor cells to treat a blinding corneal disorder, limbal stem cell deficiency (LSCD).
Corneal diseases are the second leading cause of treatable blindness in the world and more than 3.2 million people worldwide go blind from corneal diseases. LSCD has been recognized as a major cause, either primary or secondary, of significant visual loss and blindness in many common corneal disorders, such as chemical/thermal burn, keratopathy related to contact lens wear and severe infection and inflammation.
Deng hopes to develop new cell engineering methods that can efficiently expand and regenerate patient –specific limbal stem cells using a contamination-free system to generate enough cells for transplantation. The first goal is to establish the contamination-free culture system by replacing the mouse feeder cells traditionally used to expand and regenerate the limbal stem cells with a human feeder system. Deng hopes to then further optimize the expansion efficiency of her system by modulating the Wnt and Notch cell signaling pathways, which regulate the proliferation and differentiation of corneal epithelial cells. In parallel, she hopes to reprogram human skin epithelial stem cells into corneal epithelial cells using a similar approach. The ability and safety of these regenerated human corneal epithelial stem cells to reconstruct the ocular surface of the eye will be tested in a LSCD animal model.
In his study, Havton will focus on possible treatments for injuries to the anatomically lowest part of the spinal cord, the lumbosacral portion. Injuries to that part of the spinal cord are associated with paralysis, loss of sensation, severe pain and loss of bladder, bowel and sexual function. Havton hopes to determine whether immediate transplantation of human embryonic stem cells that have been directed to form motor neurons that resemble those normally associated with the lumbosacral spinal cord may replace lost nerve cells and result in a return of bladder function in an animal model of lumbosacral spinal cord injury and repair. He also hopes to determine whether delayed transplantation of human embryonic stem cells that have been directed to form motor neurons that resemble those normally associated with the lumbosacral spinal cord may replace lost nerve cells and result in a return of bladder function in an animal model.
Havton will perform a variety of functional studies to determine the effect of the cell transplantation on bladder function, walking and pain. He also will use detailed anatomical studies to determine whether the transplanted cells have grown processes to connect with pelvic target tissues, including the lower urinary tract. If successful, the proposed experiments may lead to a new treatment strategy for patients with lumbosacral spinal cord injuries, which represent approximately one-fifth of all traumatic lesions to the human spinal cord.
The success of all three projects will provide the basis for investigational new drug applications to the FDA and the initiation of human clinical trials.
To date, scientists with the UCLA Broad Stem Cell Center have received 40 CIRM grants totaling more than $135 million.