Controlling the hormonal environment in endometrial cancer sensitizes tumors to PARP inhibitors
Modulating the hormonal environment in which endometrial cancers grow could make tumors significantly more sensitive to a new class of drugs known as PARP inhibitors, UCLA researchers have shown for the first time.
The findings could lead to a novel one-two punch therapy to fight endometrial cancers and provide an alternative option for conventional treatments that, particularly in advanced disease, have limited efficacy.
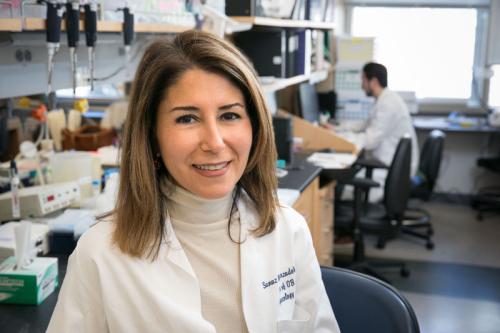
Studies on endometrial cancer cell lines have shown that PARP inhibition induces cell death when tumor suppressor PTEN is missing, a defect found in about 80 percent of human endometrial cancers. However, the UCLA researchers wanted to test the inhibitors in a laboratory model with a tumor microenvironment that closely resembles human endometrial cancer to see if this therapy would be effective, said study senior author Dr. Sanaz Memarzadeh, an assistant professor of obstetrics and gynecology and director of the G.O. Discovery Lab at UCLA.
The study appears Nov. 12, 2013 in Molecular Cancer Therapeutics, a peer-reviewed journal of the American Association for Cancer Research.
“A PARP inhibitor was given orally in two hormonal extremes – high and low estrogen,” Memarzadeh said. “The treatment achieved a significant reduction in tumor size in a low estrogenic milieu. In striking contrast, no response to the inhibitor was seen in tumors exposed to high levels of estrogen.”
The G.O. Discovery research team began their work testing PARP inhibitors in endometrial cancer after clinical testing in breast and ovarian cancers showed that the drugs were only harmful to cells if they had a defect in DNA double strand repair, which is common in some cancers, said Dr. Daniel Paik, a third year fellow in gynecologic oncology.
The BRCA gene mutations that can cause breast and ovarian cancers interfere with the cell’s DNA homologous recombination repair pathway. PTEN mutation or deletion is also thought to cause DNA damage by interfering with this cell signaling pathway.
“We wanted to see if the inhibitors were effective in endometrial tumors that had PTEN loss, on the premise that PTEN is involved in DNA repair and its loss interfered with this process,” Paik said. “In our experiments, we found that tumors treated with the inhibitors did show decreased growth, but that this did not rely solely on the loss of PTEN.”
So what was happening?
Deanna Janzen, a senior scientist in the G.O. Discovery Lab, said that endometrial cancer is associated with obesity, and fat cells in the body act as mini factories for estrogen production by converting androgens into estrogen, creating an estrogen-heavy environment.
“Because of that, we decided to first test the effectiveness of the inhibitors in a high-level estrogen environment,” Janzen said. “Much to our surprise, these PTEN-null tumors did not respond at all. It was as if we hadn’t given any PARP inhibitors.”
Memarzadeh said they repeated the experiment and did not administer estrogen, creating a low-level hormonal environment. They saw a dramatic response, with the tumors shrinking significantly. The team, along with collaborators at UCLA, found that estrogen levels affected the metabolism of the PARP inhibitor. A low estrogen environment resulted in a significant increase in the amount of drug detected in the blood stream and available to fight the cancer. A high estrogen environment resulted in less drug circulating in the system, but they could still detect evidence of drug activity in the tumor. Circulating drug levels alone could not explain what they were seeing, so they dug deeper.
The team further found that tumors in high estrogen environments were better able to repair DNA damage, which caused resistance to the effects of PARP inhibition. Estrogen supplemented tumors expressed higher levels of proteins capable of repairing the DNA, Memarzadeh said. In a low estrogen environment, decreased levels and function of the DNA repair proteins were found, allowing PARP inhibitors to induce tumor cell death.
“This study showed us that endometrial cancers that have defects in PTEN are sensitive to PARP inhibition, but the response hinges on low levels of estrogen,” Memarzadeh said. “And we learned that the hormonal milieu may significantly impact tumor response to this therapy. The difference in the response was remarkable. It was like night and day.”
The UCLA team studied endometrial cancer, but their finding may be relevant in other hormone-driven cancers, such as breast, prostate and ovarian tumors, Memarzadeh said.
Going forward, the G.O. Discover Lab team hopes to translate their findings from bench to bedside. They would like to see clinical trials launched in endometrial cancer patients who have PTEN mutations, treating them with PARP inhibitors and estrogen modulating agents.
Endometrial cancer, which starts in the endometrium or the inner lining of the uterus, is the most common gynecologic cancer in the United States. About 49,000 new cases of endometrial cancer will be diagnosed this year alone, and about 8,000 American women will die from their cancers.
The study was funded by the Concern Foundation, National Cancer Institute (U54-CA-143931), UCLA’s Scholars in Translational Medicine Program, Mary Kay Foundation, STOP Cancer, Broad Stem Cell Research Center Research Award, Sidney Kimmel Foundation, National Center for Research Resources (UL1TR000124) and the University of California Research Coordinating Committee.
“Results of this pre-clinical trial suggest that orally administered PARP inhibitors in a low estrogenic hormonal milieu can effectively target PTEN-null endometrial tumors,” the study states. “Extension of this work to clinical trials could personalize the therapy of women afflicted with advanced endometrial cancer using well tolerated orally administered therapeutic agents.”
